Effective bone stabilization is essential in orthopedics. One popular method involves the use of "nail intramedullari." This surgical technique offers a reliable solution for fractures. It provides internal support within the bone. The intramedullary nail is placed in the medullary cavity of the bone.
Surgeons must consider several factors during this procedure. Proper alignment and fixation are crucial. Surgeons also need to assess the type and location of the fracture. Sometimes, achieving optimal stabilization can be challenging. There may be complications like infection or improper nail positioning. These issues require careful attention and planning.
Using Nail Intramedullari effectively can significantly enhance patient outcomes. However, mistakes can happen. Continuous learning and adaptation are necessary for improvement. Surgeons need to reflect on past cases to refine their techniques. This approach not only aids in healing but also encourages growth in surgical practices.
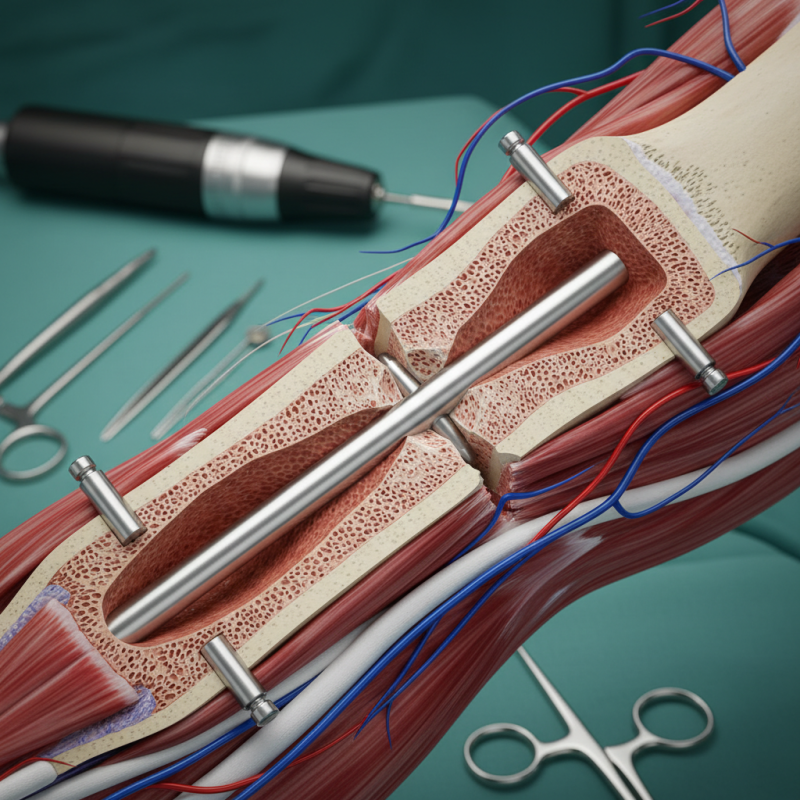
Nail intramedullari, also known as intramedullary nails, plays a critical role in bone stabilization. This method is often used for treating fractures in long bones. The nail is inserted into the medullary cavity. It helps in aligning the fractured parts, promoting healing.
A key benefit of nail intramedullari is its minimal impact on surrounding tissues. Surgeons typically perform the procedure using a small incision. This leads to less postoperative pain and quicker recovery. However, precision is crucial. Misalignment during insertion can complicate healing. Surgeons must be vigilant during this step.
Despite its advantages, the technique is not without challenges. Complications may arise, such as infection or malunion. Continuous research is needed to improve outcomes. Understanding the nuances of nail intramedullari can enhance surgical success. Each case demands careful evaluation and skill.
Intramedullary nails are a significant advancement in orthopedic surgery. They stabilize long bone fractures effectively. Indications for their use include femoral, tibial, and humeral fractures. These nails are particularly useful in cases where other techniques fail. Studies show they reduce healing time by 20-30%.
In complex fractures, intramedullary nails provide the necessary stability. They allow for early mobilization. However, improper placement can lead to complications. About 10% of patients experience issues like malalignment or infection. Surgeons must assess patient needs meticulously before deciding. A tailored approach enhances outcomes.
Additional indications for intramedullary nails include pathological fractures and non-unions. In these cases, they can support weakened bones effectively. Still, there’s a risk of over-reliance on this technique. Continuous evaluation of patient progress is vital. The balance between intervention and natural healing needs careful consideration.
Intramedullary nailing is a common method for stabilizing long bone fractures. This technique involves inserting a metal rod into the medullary cavity. It provides alignment and immobilization. The success rate for this method is impressive, with studies showing over 90% of patients achieve good to excellent outcomes.
Surgical techniques vary based on fracture types. Closed nailing is often preferred to minimize soft tissue damage. In some cases, reaming the canal is vital. This step increases the chances of bone healing. However, not every surgeon uses this technique due to potential complications like thermal necrosis. Alongside this, it is crucial to ensure proper nail size and alignment during insertion. Multiple studies indicate that misalignment can lead to malunions and impaired function.
Surgeons must consider patient-specific factors. Bone quality and age influence surgical outcomes. For instance, elderly patients tend to have poorer healing rates. Observing patient reactions during the procedure is also essential. Some patients report pain post-surgery, which can affect rehabilitation. Ongoing reflection on these varying outcomes is necessary to refine techniques and enhance patient care.
Postoperative care is crucial after an intramedullary nailing procedure. Proper management can significantly improve recovery outcomes for patients with fractures. Studies show that about 15% of patients experience complications like infection or delayed healing. Effective rehabilitation strategies can mitigate these risks.
One essential aspect is early mobilization. Patients should begin gentle movements within a week post-surgery. This approach helps maintain joint flexibility and muscle strength. Physical therapy often starts with range-of-motion exercises. Research indicates that patients who engage in early rehabilitation have a 30% faster recovery rate.
Monitoring is equally important. Surgeons emphasize the need for regular follow-up appointments. These visits allow for timely intervention if complications arise. Unfortunately, not all patients adhere to this guidance, leading to potential setbacks. Reflection on one's recovery journey is vital. It helps identify areas needing focus or improvement. Each patient’s experience is unique, highlighting the need for personalized rehabilitation plans that consider individual progress and challenges.
Intramedullary nailing is widely used for bone stabilization, but complications can arise. According to the Journal of Bone and Joint Surgery, complications occur in approximately 15-25% of cases. These can include infection, nonunion, and malalignment. Surgeons must be prepared to manage these issues effectively.
Infection is a notable risk, particularly when there is skin involvement. A study published in Clinical Orthopaedics and Related Research found that superficial infections occur in up to 12% of patients. Proper sterile techniques and post-operative care can significantly reduce this rate. Immediate identification of infection signs, like redness or swelling, is crucial.
Nonunion and malalignment are other challenges. These complications may result from improper nail positioning or inadequate healing. A review in the Journal of Orthopaedic Trauma highlights that 5-10% of fractures fail to unite. Continuous assessment through imaging is important. Surgeons should be vigilant for any signs of failure to heal and be ready to adjust treatment plans as necessary.